Georgia
Emergency Preparedness Coalition
for
Individuals with Disabilities and Older Adults
American
Red Cross of Georgia (ARC) Atlanta Autism Consortium
Center
for Advance Communication Policy, Georgia Institute of Technology
DeKalb
Emergency Management Agency (DEMA) Federal Emergency Management Agency (FEMA)
Friends of Disabled Adults and Children (FODAC) GACHI, Serving the Deaf &
Hard of Hearing Georgia Advocacy Office (GAO)
Georgia
Department of Behavioral Health and Developmental Disabilities
(DBHDD)
Georgia
Department of Human Services, Division of Aging Services (DAS) Georgia
Department of Human Services, Office of Facilities and Support Services (OFSS)
Georgia
Department of Public Health, Division of Health Protection, Office of
Emergency Preparedness and Response (DPH) Georgia
Emergency Management Agency (GEMA)
Georgia
Emergency Management Interpreting Initiative (GEMINI) Georgia State Financing
and Investment Commission-
State
ADA (Americans with Disabilities Act) Coordinator's Office
Gwinnett
Coalition Emergency Preparedness Committee
Gwinnett,
Newton and Rockdale County Public Health Department, Office of
Emergency
Preparedness Joseph’s Network Shepherd Center
Southeast
ADA Center
Tools
for Life, Georgia’s Assistive Technology Act Program
Funding
for this tips guide provided by:
Georgia
State Financing and Investment Commission
State
ADA Coordinator's Office
The
Georgia Emergency Preparedness Coalition
for
Individuals with Disabilities and Older Adults would like to thank the original
creators and publishers of this tips guide:
Center for Development and Disability, University of
New Mexico
New Mexico Department of Health,
Office of Health, Emergency Management
American Association on Health
& Disability American Association on Health & Disability
New Mexico Governor's Commission on
Disability Research and Training Center on Independent Living
The
State of Texas Functional Needs
Support
Services Integration Committee
The
Oklahoma Developmental Disabilities Council
Dear First
Responder:
Emergencies are
stressful enough, but they may be especially traumatic
for
individuals with disabilities. As a first responder, you must consider the
unique needs of people with disabilities in an emergency.
Some
disabilities are easily identifiable, while others may be less apparent to a
casual observer.
This
quick reference guide provides specific, practical tips for working with people
who have a wide range of disabilities. The information is color-coded for easy
access before, during, and after a crisis.
Remember,
as a first responder, people depend on you to provide critical assistance when
they are most vulnerable. Hopefully, this information will help you assist the
individuals you serve during an emergency.
For
more information about how to assist people with disabilities, refer to the
resource section at the back of this guide. Thank you for what you do, and for
taking the time to review this information.
Sincerely,
Georgia
Emergency Preparedness Coalition for Individuals with Disabilities and Older
Adults
■ Be
respectful and courteous when working with individuals with
disabilities and
older adults.
■
When introduced to a person with a disability, it is appropriate to offer to
shake hands. People with limited hand use or an artificial limb can usually
shake hands (Shaking hands with the left hand is an acceptable greeting).
■ If you
offer assistance, wait until the offer is accepted, then listen to
or ask for
instructions.
■
Do not use first names unless requested to do so by the person you are
assisting.
■
Relax. Do not be embarrassed if you happen to use common expressions such as
"See you later," or "Did you hear about that?" that seem to
relate to a person's disability.
■ Do not be
afraid to ask questions when you are unsure of what to do.
■
Upon arrival, ask or look for an identification bracelet with special health
information, essential equipment and supplies, medication, mobility aids,
special communication information, signs of stress and/or confusion, and
emergency contact information to reach the person's family. By being prepared
and observant before you offer help to an individual in distress, you may
reduce the person's stress and confusion during an emergency.
Always
ask Older Adults how you can best assist them.
■ Older Adults may respond slowly to a crisis and may not fully
understand the extent of the emergency. Repeat questions and answers if
necessary. Be patient!
■ Older Adults may fear being
placed in a nursing facility against their will. Assure them they are merely
receiving medical treatment, not being taken to a nursing or care facility.
■ Older Adults may fear being
removed from their homes. Explain that this relocation is most likely
temporary.
■ Before moving older people,
assess their ability to speak, see and hear; adapt rescue techniques for
sensory impairments.
■ Older Adults with a hearing
loss may appear disoriented and confused when in reality they cannot hear you.
Determine if the person has a hearing aid. If they do, is it available and
working? If it
is not, can you
get a new battery to make it work? See the tip sheet for
People Who Are
Deaf or Hard of Hearing for more information.
■ If the person has vision
loss, identify yourself and explain why you are there. Offer the person your
elbow as a guide to moving them to safety; otherwise speak continuously while
they follow you to safety. Let the person hold your arm and then guide them to
safety. See the tip sheet for People Who Are Blind or Have Visual Difficulties
for more information.
■ Ask the person what
medications they are taking and where their medications are stored. If
possible, gather all medications before evacuating. Most people keep all their
medications in one location in their homes. If they cannot bring their
medications, ask if they have
a list of their
medications, an emergency contact number for their
health care
provider(s) and their family emergency contact.
■ If the person is disoriented
or not responding to you, they may have dementia or be in shock. Turn off
emergency lights and sirens if possible. Identify yourself and explain why you
are there. Speak slowly and calmly, using short words. Ask "yes" or
"no" questions, and repeat them if necessary. Maintain eye contact.
Traditionally, the term "service animal" referred to
seeing-eye dogs. However, now a service animal is a dog that is individually
trained to do work or perform tasks for a person with a disability. Examples of such work or tasks include guiding people who are
blind, alerting people who are deaf,
pulling a
wheelchair, alerting and protecting a person who is having a seizure, reminding
a person with mental illness to take prescribed medications, calming a person
with Post Traumatic Stress Disorder (PTSD) during an anxiety attack, or
performing other duties.
In addition, there is a special provision for miniature horses
under the ADA and entities covered by the ADA must modify their policies to
permit miniature horses where reasonable.
For
more information on persons with disabilities who use service animals, see ADA
2010 Revised Requirements: Service Animals at www.ada.gov/service_animals_2010.html
■
Remember - a service animal is not a pet. Service animals are
allowed
to go anywhere a person could go, including food preparation and medical areas.
■ Do not touch or give the
animal food or treats without the permission of the owner.
■ When a dog is wearing its
harness, it is on duty. If you are asked to take the dog while assisting the
individual, hold the leash and not the harness.
■ A service animal is an extension
of the person who uses it. These animals should be evacuated with the person
who uses it.
■ Service animals are not registered and there is no proof that the
animal is a service animal. If the person tells you it is a service animal,
treat it as such. If you have doubts, provide care and service first. When you
arrive at your destination, address the issue with the supervisor in charge.
■ If the animal is out of
control or presents a threat to the individual or others, first let the owner
attempt to control the animal; if this is unsuccessful, remove it from the
site.
■ A person is not required to
give you proof of a disability that requires a service animal. You must accept
that he or she has a disability.
■ People with psychiatric and
emotional disabilities may have a companion animal. Although companion animals
are not considered service animals under the ADA Amendments, these animals can
be just as important to the individuals as a service animal is to an individual
with a physical disability.
■ Service animals must be
harnessed, leashed, or tethered, unless these devices interfere with the service
animal's work or the individual's disability prevents using these devices.
■ Every effort should be made to ensure the service animal is evacuated
with the person.
■
Refer to the section in this Tips Guide on People with Service Animals.
A
mobility device (e.g. wheelchair, walker, etc.) is an extension of the person
who uses it. These devices should be evacuated with the individual. However, if
it is impossible to evacuate an individual's wheelchair, please make every
effort to bring the wheelchair transfer board and/or seat cushion. (Note: For
individuals who use upper floors, an evacuation (stair) chair or similar device
may need to be provided).
■ Always ask the
person how you can help before attempting to assist. Even when there is an
urgent need to evacuate, respect their independence. Do not make assumptions
about the person's abilities.
■
Ask if they have limitations or problems that may affect their
safety.
■ Some people may need
assistance getting out of bed or out of a chair, but can then
proceed without assistance. Ask!
■
Here are some questions you may find helpful:
o "Are you able to stand
or walk without the help of a mobility device like a cane, a walker or a
wheelchair?"
o "You might have to [stand] [walk] for quite a while on your
own. Will this be all right? Please be sure to tell someone if you think you
need assistance."
o "Are
you able to use your arms?"
■ When carrying people, avoid putting pressure on their arms, legs
or chest. This may cause spasms or pain, and may even interfere with their
ability to breathe.
■ If possible, avoid using the
fireman's carry. Use the one-person or two-person carry technique.
Crutches, Canes
or Other Mobility Devices:
■ A person using a mobility
device may be able to negotiate stairs independently. One hand is used to grasp
the handrail while the other hand holds the crutch or cane. Do not interfere
with the person's movement unless you are asked, except when absolute speed is
the primary concern. If this is the case, tell the person what you will need to
do and why.
■
Offer to carry the extra crutch.
■ If the stairs are crowded,
act as a buffer and run interference for the person.
Evacuating People
Who Use Wheelchairs:
■ If the conversation will
take more than a few minutes, sit down to speak to the person at eye level.
■ People who use wheelchairs
are trained in special techniques to transfer from one chair to another.
Depending on their upper body strength, they may be able to do much of the work
themselves.
■ Do not assume you need to
help, or presume to know what kind of help to give. Ask first.
Non-Motorized
Wheelchairs:
Whenever
possible, the in-chair carry is the most desirable technique to use.
■
One-person assist. The rescuer should assume
the following
position:
■
Grasp the pushing grips, if available.
■
Stand one step above and behind the wheelchair.
■
Tilt the wheelchair backward until a balance (fulcrum) is
achieved.
■
Keep your center of gravity low.
■
Descend frontward.
■
Let the back wheels gradually lower to the next step.
■ Two-person assist. The first rescuer should assume the position described in the one-person assist. The second rescuer should:
■
Stand in front of the wheelchair and face the wheelchair.
■ Stand one, two, or three
steps down (depending on the height of the other rescuer).
■
Grasp the frame of the wheelchair.
■
Push into the wheelchair.
■
Descend the stairs backwards.
Motorized
Wheelchairs:
■ Motorized wheelchairs may
weigh as much as 400-500 pounds unoccupied, and may be longer than manual
wheelchairs. Lifting a motorized wheelchair and user up or down stairs requires
two to four people.
■ People in motorized
wheelchairs probably know their equipment much better than you do! Before
lifting, ask about heavy chair parts that can be temporarily detached; also ask
how you should position yourselves, where you should grab hold and at what
angle, if any, to tip the chair backward.
■
Turn the power to the wheelchair off before lifting it.
■ Many people who use
motorized wheelchairs have limited arm and hand motion. Ask if they have any
special requirements for being transported down the stairs.
■ There is a difference
between the terms "hard of hearing" and "deaf." People who
are hard of hearing vary in the extent of hearing loss they experience. Some
are completely deaf, while others can hear almost normally with hearing aids.
■ Hearing aids do not
guarantee that the person can hear and understand speech. They increase volume,
not necessarily clarity.
■ If possible, flick the
lights when entering an area or room to get the individual's attention.
■ Establish eye contact with
the individual, not with the interpreter, if one is present.
■
Use facial expressions and hand gestures as visual cues.
■ Make sure the person
understands you and repeat what you said if necessary.
■ Offer pencil and paper.
Write slowly and let the individual read as you write.
■ Written communication may be
especially important if you are unable to understand the person's speech.
■ Do not allow others to
interrupt you while conveying the emergency information.
■ Be patient - the person may
have difficulty understanding the urgency of your message.
■ Provide people with a flashlight to signal their location if they
are separated from the rescue team. This will facilitate lip-reading or signing
in the dark.
■ While written communication
works for many people, others may not understand English well enough to
understand written instructions. Keep instructions simple, in the present tense
and use basic vocabulary.
Work
with your local deaf and hard of hearing community and consider the
communication tools and techniques below:
High Tech
Communication tools:
■
Utilize hand held mobile devices to text back and forth.
■
Deliver general announcements via text blast or email.
■ Share a computer to
facilitate written communication. (Utilize large font for individuals who
have visual loss)
■ Establish Video Remote
Interpreting (VRI) services which may be used to provide effective
communication. VRI is an interpreting service that uses video conference
technology over dedicated lines or that uses wireless technology with a
high-speed, wide-bandwidth video connection that delivers high-quality video
images.
■ Utilize accessibility tools
that individuals may bring with them for communication.
Low Tech
Communication tools:
■
Utilize pen and paper to clearly and legibly print information.
■ White boards with large font
to carry through the shelter area with announcement information.
■
Should this be for Blind or vision loss or Deaf-Blind:
■ Print general instructions
in large print (minimum font size of 18 points) and in Braille.
■ Record announcements or
information on tapes or other data and provide access to mediums to listen to
the materials.
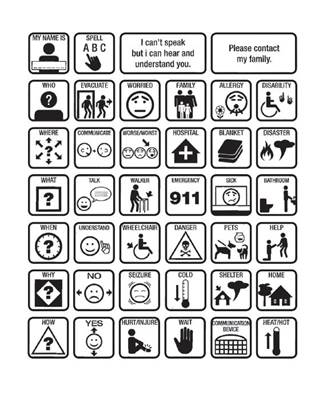
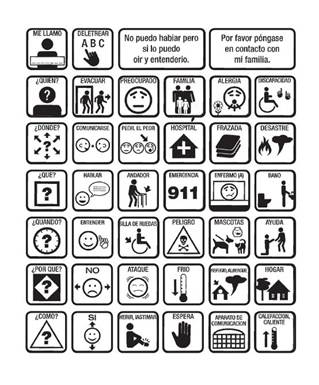
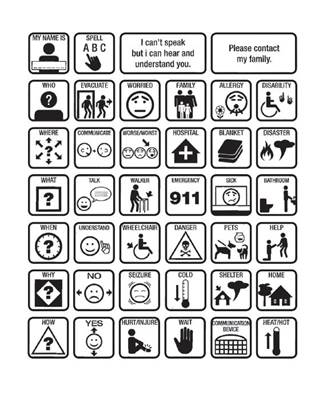
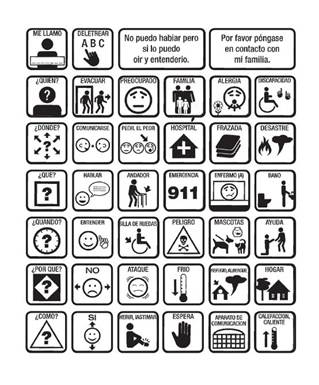
■ Utilize American Red Cross
"Visual Language Translator for Emergency Assistance" booklet,
"Language Identification Chart", "Basic Emergency Sign Language
Poster" Braille communication book and pictogram tools.
Provide for an
onsite American Sign Language (ASL) Interpreter:
Although
various technological methods are available for communicating with persons who
are deaf, the circumstances of an emergency can incapacitate these methods or
reduce their effectiveness. In adverse situations, sign language interpreters
can be a very effective communication link with deaf persons and those who may
depend on lip reading. Effective communication can best be assessed by asking
the individual which communication methods work for them.
Understanding
American Sign Language:
American
Sign Language (ASL) uses visually transmitted sign patterns to convey meaning
while simultaneously combining hand shapes, body orientation and movement of
the hands, arms or facial expressions to fluidly express a speaker's thoughts.
In terms of sentence structure, people who
use ASL and have
been deaf from birth, use topic-comment syntax, while
hearing people
who speak English use subject-object-verb. Speakers of sign language
communicate through concepts and words in non-English sentences.
While
it is possible to interpret sign language into a spoken language such as
English (and vice versa), such an interpretation often is not a direct
translation. American Sign Language (ASL) is a complex visual-spatial language
that is used by the community who is deaf in the United States. It is a
linguistically complete, natural language. It is the native language of many
men and women who are deaf, as well as some hearing children
born into
families of parents who are deaf. Sign languages across time are
developed
specific to their communities and are not universal. For example, ASL is
completely different from British Sign Language even though both countries
speak English.
One
example of conceptual framework for sign language would be, if an employee in a
grocery store asks his supervisor for the day before Thanksgiving off...he
would say, "Do you mind if I have the day before Thanksgiving off?
Translated into sign language would be, " Wednesday, day before
thanksgiving, don't-mind, off." Another example would be
if a person in a
shelter was asked, " How often do you need to take your
medication?"
In sign language it would conceptually translate to, "Medicine
pills-taking how many times day?"
See
Georgia Communications Options for Individuals Who Are Deaf, Hard of Hearing or
Have Speech Difficulties Guide for Additional Resources (http://ada.georgia.gov).
■ There is a difference
between visual loss and blindness. Some people who are legally blind have some
sight, while others are totally blind.
■
Announce your presence, speak out, and then enter the area.
■
Speak naturally and directly to the individual.
■
Do not shout.
■
Don't be afraid to use words like see, look, or blind.
■ State the nature of the
emergency and offer the individual your elbow as a guide. As you walk, be verbally
descriptive; advise the individual of any obstacles. Be sure to mention stairs,
doorways, narrow passages, ramps, etc.
■ Do not grab or attempt to
guide a person without first asking for permission.
■ If needed, let the person
grasp your elbow, arm or shoulder lightly for guidance.
■ A person may choose to walk
slightly behind you to gauge your body's reactions to obstacles.
■ When guiding someone to a
seat, place the person's hand on the back of the chair.
■ When leading several
individuals with vision loss, ask them to guide the person behind them.
■ Remember that you'll need to
communicate any written information orally.
■ When you have reached
safety, orient the person to the location and ask if any further assistance is
needed.
■ Give the person your full
attention. Listen patiently and carefully, and try not to interrupt or finish
the person's sentences.
■ Do not assume that the
person with a speech impairment does not understand you.
■ If you have trouble
understanding, ask the person to repeat the statement. If, after trying, you
still cannot understand, ask the person to write it down or suggest another way
to communicate.
■ If necessary, repeat a
statement in order to clarify or confirm what the person said.
■ When possible, provide a
quiet environment to make communication easier.
■ If a person begins to
exhibit unusual behavior, do not assume they have a mental health condition.
Unusual behavior can be caused by extreme emotion, stress or physical
conditions such as lack of oxygen, low blood sugar, or diabetes.
■ You may not be able to tell
if a person has a mental health condition. They may cope well under routine
conditions but the stress of an emergency may cause them to decompensate or
have a sudden loss of control.
■ If you suspect someone has a
mental health condition, use the following tips to help you through the
situation:
■ In an emergency, the person
may become confused. Speak slowly in a normal, calm tone.
■
Do not talk down to them; do not yell or shout.
■
Lean forward—this shows interest and concern.
■ If the person becomes
agitated, help them find a quiet corner away from the confusion.
■
Keep your communication simple, clear and brief.
■ If they are confused, do not
give multiple commands—ask or state one thing at a time.
■ Be sympathetic—show that you
have heard them and care about what they have told you. Be reassuring.
■ If the person is delusional,
do not try to talk the person out of it. Just let them know you are there to
help.
■
Ask if there is any medication they should take with them.
■ Try to avoid interrupting
the person who might be disoriented or rambling—just let him or her know that
you have to move quickly.
■ People with psychiatric and
emotional disabilities may have a companion animal. Although companion animals
are not considered service animals under the ADA, these animals can be just as
important as a service animal is to a person with a physical disability.
Say:
■
My name is… "I am here to help you, not hurt you."
■
I am a … (name your job).
■
I am here because … (explain the situation).
■ I look different than my picture on my badge because… ( for
example, if you are wearing protective equipment).
Show:
■
Your picture identification badge (as you say the above).
■
Calmness and ability to do your job.
■ Respect for the dignity of the person (example: speak directly
to the person).
Give:
■ Extra time for the person to
process what you are saying and to respond.
■ An arm to the person to hold
as they walk, if needed. Offer your elbow for balance.
■
Quiet time to rest, if at all possible, to lower stress and
fatigue.
Use:
■
Short sentences.
■
Simple, concrete words.
■
Accurate, honest information.
■
Pictures and objects to illustrate your words.
■ Point to your ID picture as
you say who you are; point to any protective equipment as you speak about it.
*
A cognitive disability affects a person's ability to reason, understand, and
learn. Cognitive disabilities are sometimes referred to as intellectual
disabilities.
Predict:
■
What will happen (simply and realistically).
■ When events will happen (tie
to common events in addition to numbers and time, for example, "By lunch
time…" "By the time the
sun goes down…").
■ How long this will last—when
things will return to normal (if you know).
■ When the person can contact
or rejoin loved ones (for example: calls to family, reuniting with pets).
Ask for/Look for:
■
An identification bracelet with special health information.
■ Essential equipment and supplies (for example, wheelchair, walker,
oxygen, batteries, Communication devices [head pointers, alphabet boards,
speech synthesizers, etc.]).
■
Medication.
■
Service animal.
■
Special health instructions (for example, allergies).
■ Special communication
information (for example, is the person using sign language or other assistive
technology).
■
Contact information.
■ Signs
of stress and/or confusion (for example, the person might say he or she is
stressed, look confused, withdraw or start rubbing his or her hands together).
■ Conditions that people might
misinterpret (for example, someone might mistake Cerebral Palsy for
drunkenness).
Repeat:
■ Reassurances (for example,
"You may feel afraid. That is all right. We are safe now.").
■ Encouragement (for example,
"Thanks for moving fast. You are doing great. Other people can look at you
and know what to do.").
■ Frequent updates on what is
happening and what will happen next. Refer to what you predicted will happen,
for example: "Just like I said before, we are getting into my car now. We
will go to … now. "
Reduce:
■ Visual and Auditory
Distractions. For example, lower the volume of a radio, use flashing lights and
sirens on a vehicle only when necessary.
Explain:
■
Any written material (including signs) in everyday language.
■
Public address system announcements in simple language.
Share:
■ The information you have
learned about the person with other workers who will be assisting.
Communication:
■ Speak calmly. Use direct,
concrete phrases with no more than one or two steps, or write brief
instructions on a pad if the person can read.
■
Allow extra time for the person to respond.
■
The person may repeat what you said, repeat the same phrase,
talk
about topics unrelated to the situation, or have an unusual or monotone voice.
This is their attempt to communicate, and is not meant to irritate you or be
disrespectful.
■ Avoid using phrases or slang
that have more than one meaning such as "spread eagle" "knock it
off" or "cut it out".
■ Visually check to see if
there is a wrist or arm tattoo or bracelet that identifies the person as having
an autism spectrum disorder.
■ Some people with autism may
not indicate they are experiencing pain-check for injuries.
Social:
■
Approach the person in a calm, non-threatening manner.
■ The person may not
understand typical social rules or read social clues. He or she may be dressed
inappropriately, enter your personal space, prefer to be farther away from you,
or may not make eye contact.
■ The person may have unusual
facial expressions or laugh or giggle inappropriately, or may have difficulty
understanding the seriousness of the situation. Do not interpret these
behaviors as deceit or disrespect.
■ Because of the difference in their social understanding, persons
with autism may display behaviors that are misinterpreted as evidence of drug
abuse or psychosis, defiance or belligerence. Do not assume!
Sensory and
Behavior:
■
If possible, turn off sirens, lights, and remove canine partners.
Attempt to find a
quiet location for the person, especially if you need to talk with the
individual.
■ Avoid touching the person,
and if necessary, gesture or slowly guide the person .
■ If the person is showing obsessive or repetitive behaviors, or is
fixated on a topic or object, avoid stopping these behaviors or removing the
object unless there is risk to self or others.
■ Make sure that the person is
away from potential hazards (busy streets, etc.) because the individual may not
have a fear of danger.
■ Be alert to the possibility
of outbursts or impulsive, unexplained behavior. If the person is not harming
anyone, wait until these behaviors subside.
People
with chemical sensitivities people can become ill from exposure to a wide
variety of chemicals at levels that others may not be able to detect. They may
lose their ability to think, speak or follow directions. If a person is having
difficulty in communicating or appears unusually irritable, agitated or
distraught, ask the person if she/he has chemical sensitivities.
Initial Tips:
■ If a person says that she or
he is being made sick by an exposure, accept what the person is saying and ask
what she or he needs.
■ Assure the person that you
understand and will work with providing care or direction. Ask the person what
triggers the negative reactions (example: medications, cleaning products,
perfumes, etc.).
■
Do not idle ambulance or other emergency vehicle engines.
■ Move the person to an area with
the cleanest air possible - outdoors is frequently helpful.
■ Try not to use latex
gloves, disinfectants, cleaners or other sprays or products near a person who
has chemical sensitivities.
In a shelter:
■ Assign caregivers who are
not wearing perfume, cologne, aftershave or other scented products such as
fabric softeners and who do not smoke.
■ Avoid rooms with recent
pesticide sprays, strong scented disinfectants or cleaners, new paint or carpet
or other recent remodeling.
■ Allow a person who has chemical
sensitivities to use or bring their own masks, air filters, oxygen tubing,
supplements, medications,
food, water,
clothing and other medical supplies.
If you administer
drugs:
■
Administer low doses with caution.
■
Use IV fluid bottled in glass without dextrose if possible.
■ Capsules are generally
better than tablets - they have fewer binders, fillers and dyes.
■
If administering anesthesia, use short-acting regional rather
than
general anesthesia wherever possible and try to avoid use of halogenated gas
anesthetics.
Individuals
who are Deaf-Blind have combined hearing and vision loss. Individuals may be
Deaf-Blind, deaf with low vision, or hard of hearing with any kind of vision
loss.
■ Let the person know you are
there by simple touch on the shoulder or arm.
■
Avoid bright/glaring and loud environments.
■
Identify yourself.
■ Communicate directly with
the person, even when using an interpreter.
■ Do not assume the person
knows where she or he is or what is going on. Share as much information as
possible.
■ Always tell the person when
you are leaving, even if it is for a brief period of time. Leave the person as
comfortable and safe as possible. It is good to offer a chair, table, or wall
for an anchor.
■ When guiding the person,
never place him/her ahead of you. Allow the person to hold your arm above the
elbow. It is rarely necessary to "help" the deaf-blind person sit
down or climb stairs; placing their hand on a chair or banister will give them
the information they need.
Communication:
People who are
deaf-blind sometimes have usable speech, vision and/
or
hearing. Determine if the individual can effectively communicate via speech,
American Sign Language (ASL), finger spelling, writing with a
dark
pen, computer or assistive communication device or print-on-palm. If a citizen
who is deaf-blind indicates that they are in need of Sign Language assistance
for effective communication, attempt to determine which sign language modes
used by people who are deaf-blind provide for their needs. Coordinate with
Interpreter providers to ensure that Interpreters with the appropriate skills
are requested .
Georgia
Emergency Preparedness Coalition for Individuals with
Disabilities
and Older Adults Contact List
American
Red Cross of Georgia:
Phone:
(404) 876-3302 to reach your local chapter,
Website:
www.redcross.org, select "Disaster Services"
then "Be Prepared"
Atlanta
Autism Consortium:
Website:
www.atlantaautismconsortium.com
Center
for Advanced Communications Policy-Georgia Institute of Technology:
Phone:
(404) 385-4614, Fax: (404) 385-0269, Website: www.cacp.gatech.edu/
Dekalb
County Emergency Management Agency (DEMA):
Phone:
(770) 270-0413,
Website:
http://web.co.dekalb.ga.us/dk_police/pol-dema.html
Federal Emergency Management Agency - (FEMA): Phone:
(770) 220-5200, Fax: (770) 220-5230, Website: www.fema.gov
Friends
of Disabled Adults and Children:
Phone:
(770) 491-9014, Toll free: 1(866) 977-1204, Fax: (770) 491-
0026, Website: www.fodac.org
GACHI-
Serving the Deaf and Hard of Hearing:
Video
Phone: (886) 250-8711, Voice/TTY: (404) 292-5312,
Voice/TTY
Toll Free: (800) 541-0710, Fax: (404) 299-3642, Website: www.gachi.org
Georgia
Advocacy Office:
Phone: (404) 885-1234 or Voice or TDD: 1(800)
537-2329, Fax: (404) 378-0031, Website: www.thegao.org
Georgia Department of Behavioral Health
and Developmental Disabilities (DBHDD):
Phone:
(404) 657-2252, Fax: (404) 657-1137, Website: www.dbhdd.georgia.gov
Georgia
Department of Human Services, Division of
Aging
Services:
Phone: 1(866) 55-AGING (552-4464),
Fax: (404) 657-5285, Website: www.aging.dhr.georgia.gov
Georgia
Department of Human Services, Office of Facilities and
Support
Services:
Phone: (404) 651-6316 (Constituent Services
Section), Website: www.dhs.georgia.gov
Georgia Department of Public Health, Division of
Health Protection, Office of Emergency Preparedness and Response (DPH): Phone:
(404) 657-2700, Fax: (404) 463-5395,
Website: www.health.state.ga.us
Georgia Emergency
Management Agency (GEMA):
Phone:
(404) 635-7000 or 1(800) TRY-GEMA (in Georgia only), TTY: (404) 635-7258, Fax: (404)
635-7005,
Website: www.gema.ga.gov/ www.ready.ga.gov
Georgia
Emergency Management Interpreting Initiative:
Phone:
(404) 537-9930, Email: educateandadvocate@gmail.com
Georgia
State Financing and Investment Commission - State ADA Coordinator's Office:
Phone:
(404) 657-7313, TTY: (404) 657-9993, Fax: (404) 463-5650,
Website:
www.ada.georgia.gov
Gwinnett
Coalition Emergency Preparedness Committee:
Phone: (770) 995-3339, Website:
www.getreadygwinnett.org
Gwinnett,
Newton, Rockdale County Health Departments:
Phone:
(770) 339-4260, Fax: (770) 339-2334, Website: www.gnrhealth.com
Joseph’s
Network:
Phone:
(404) 207-9307, Website: www.josephsnetwork.com
Shepherd
Center:
Phone:
(404) 352-2020, Website: www.shepherd.org
Southeast
ADA Center:
Toll Free Phone (Voice/TTY): 1(800)
949-4232, Phone (Voice/TTY) (404) 541-9001, Fax: (404) 541-9002,
Website:
www.adasoutheast.org
Tools For Life-The Alternative
Media Access Network, Georgia Institute of Technology Enterprise Innovation
Institute: Phone: (404) 894-0541, Toll Free: 1 (800) 497-8665,
Fax: (404) 894-
8323, Website: www.gatfl.org


Georgia
Emergency Preparedness Coalition for Individuals with Disabilities & Older
Adults
Prepare.
Plan. Stay Informed.
This
guide is available for download
on
the State ADA Coordinator's website at:
www.ada.georgia.gov